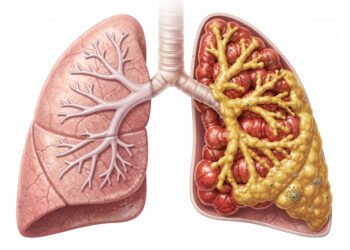
New clinical breakthroughs in drug-resistant TB treatments are offering a lifeline to the half a million people affected by this global health threat every year. Researchers have identified three innovative approaches that maintain remarkable success rates while eliminating many of the harsh side effects associated with traditional antibiotics. These drug-resistant TB treatments represent a shift from theoretical research to practical, clinical application, potentially revolutionising how the world’s most stubborn infectious disease is managed.
Why Drug-Resistant TB is Such a Pain
The Struggles We Face
Picture this: you’re a doctor in a crowded clinic in Mumbai, and the patient sitting across from you has already been through six months of standard TB treatment. The cough hasn’t improved. The night sweats continue. And when the lab results come back, they confirm your worst suspicions – the bacteria have developed resistance to at least two of the most powerful first-line drugs. Now you’re looking at a treatment plan that could stretch for 18 to 24 months, involve up to eight different medications daily, and cost upwards of $10,000 per patient.
Your patient isn’t alone in this struggle. Roughly 500,000 people develop drug-resistant TB every year worldwide, and the numbers keep climbing. What makes this particularly frustrating is that many of these cases stem from incomplete treatment courses – when patients stop taking their medications too early because they feel better, or can’t afford to continue, or simply can’t handle the brutal side effects anymore. The bacteria that survive? They’re the toughest ones, and they’re now resistant to the drugs that should’ve killed them.
Table of Contents
What Makes It So Tough to Treat?
Standard TB treatment already requires you to take multiple drugs for months on end. But when resistance enters the picture, everything gets exponentially worse. The second-line drugs used for drug-resistant TB can cause serious side effects, including permanent hearing loss, severe nausea, psychiatric problems, and kidney damage. We’re talking about medications so harsh that patients often describe the treatment as worse than the disease itself. Some of these drugs need to be injected daily for months, which means painful clinic visits and the constant risk of injection-site infections.
The success rates tell their own grim story. While regular TB can be cured in about 85% of cases, multidrug-resistant TB has historically had cure rates hovering around 50-60%. And extensively drug-resistant TB? Even lower. You’re imperatively fighting an uphill battle where the bacteria have already figured out how to survive your best weapons, and your backup options are limited, expensive, and come with a laundry list of complications that can derail treatment before it even has a chance to work.
The diagnostic challenge adds another layer of difficulty. Traditional culture-based testing for drug resistance can take weeks or even months to deliver results, and during that waiting period, patients might be on the wrong treatment regimen entirely. This delay doesn’t just affect individual outcomes – it also means people with undiagnosed drug-resistant TB continue spreading resistant strains to others in their communities. So you’ve got a situation where detection is slow, treatment is brutal and often ineffective, and transmission continues unchecked.

My Take on the Game-Changers: New Treatment Options
What’s really shaking up the TB treatment world right now isn’t just one breakthrough – it’s three completely different approaches that are actually working in real patients. After decades of watching drug-resistant TB cases climb while treatment options stayed frustratingly limited, you’re finally seeing researchers crack the code with strategies that seemed almost too simple to work. The clinical trial finds three new ways to treat drug-resistant tuberculosis that are changing how doctors approach this deadly disease.
Your biggest advantage with these new protocols? They’re cutting treatment times dramatically while reducing the pill burden that made patients want to quit halfway through. We’re talking about regimens that don’t require daily injections or leave you dealing with severe side effects for months on end. Each approach targets drug-resistant TB differently, giving your healthcare provider actual options to tailor treatment to your specific strain and circumstances.
The First Approach You Need to Know About
The six-month all-oral regimen is probably the most radical departure from traditional TB treatment you’ll encounter. Instead of the gruelling 18-24 month protocols that have been standard for multidrug-resistant TB, this approach condenses everything into half a year using a combination of newer drugs like bedaquiline and pretomanid alongside linezolid. Patients are seeing cure rates above 90% in clinical trials, which is honestly mind-blowing when you consider that conventional treatment for drug-resistant cases often failed more than half the time.
What makes this regimen so different is that it completely eliminates injectable medications – you know, those painful daily shots that left patients with hearing loss and kidney damage. Every single drug in this protocol comes in pill form, which means you can actually take your treatment at home instead of trekking to a clinic every single day. The simplicity factor alone is improving adherence rates because people aren’t abandoning treatment when the side effects become unbearable.
The Second Approach That’s Turning Heads
The nine-month standardised regimen takes a slightly different angle by using a fixed combination of drugs that works for most drug-resistant cases without requiring extensive drug sensitivity testing first. You’re getting a cocktail of medications, including moxifloxacin, clofazimine, ethambutol, and pyrazinamide that researchers have fine-tuned to hit multiple vulnerabilities in resistant TB strains simultaneously. This approach cuts your treatment time by more than half compared to the old 20-month regimens, and the standardised nature means your doctor can start you on effective treatment immediately.
The beauty of this protocol lies in its practicality for resource-limited settings where waiting weeks for lab results isn’t feasible. Instead of playing the guessing game with which drugs might work, you’re getting a proven combination that handles the most common resistance patterns right out of the gate. Clinical data show that this regimen works for about 85% of patients with multidrug-resistant TB, and when it does, people test negative for the bacteria much faster than with older treatments.
But here’s what really sets this approach apart – the side effect profile is significantly more manageable than what you’d experience with second-line injectables. Most patients report being able to maintain their daily routines and work schedules throughout treatment, which wasn’t remotely possible with the old regimens that left people bedridden or dealing with permanent disabilities. The psychological impact of knowing you’ll be done in nine months instead of nearly two years can’t be overstated – it gives you a light at the end of the tunnel that actually feels reachable.
The Third Option You Shouldn’t Ignore
The ultra-short four-month regimen is the newest kid on the block, and it’s pushing boundaries that seemed impossible just a few years ago. Using a high-dose rifapentine combined with moxifloxacin, isoniazid, and pyrazinamide, researchers discovered they could knock out drug-susceptible TB in just 16 weeks – that’s a third of the standard six-month treatment. How These Treatments Are Safe and Effective
Clinical Trial Results You Should Know About
What makes these new TB treatments different from the ones that came before? The answer lies in years of rigorous clinical testing involving thousands of patients across multiple continents. Bedaquiline, for instance, went through trials that showed it could cure up to 62% of MDR-TB patients when combined with other drugs – that’s compared to the dismal 50% success rate of older regimens. And here’s something that really matters… the side effects were significantly milder than what you’d experience with the old injectable drugs that could literally destroy your hearing.
Pretomanid’s journey through clinical trials was equally impressive. The Nix-TB trial demonstrated that when you combine it with bedaquiline and linezolid, 90% of extensively drug-resistant TB patients achieved cure – and we’re talking about people who had basically run out of options. These weren’t just numbers on paper either. Real patients who’d been sick for years finally got their lives back. The treatment duration? Six months instead of the gruelling 18-24 months that traditional regimens demanded. Delamanid showed similar promise in studies across Europe and Asia, with fewer cardiac side effects than many existing TB drugs and the ability to work against strains that had become resistant to nearly everything else in our arsenal.
Why Your Body Tolerates These Drugs Better
So what’s happening inside your body that makes these medications safer than the old guard? The new drugs work through completely different mechanisms – they target the bacteria’s energy production and cell wall formation in ways that don’t hammer your kidneys or destroy the delicate hair cells in your inner ear. Bedaquiline specifically blocks an enzyme called ATP synthase that TB bacteria need to survive, but your human cells use a different version of this enzyme that the drug doesn’t affect much. That’s why you’re not dealing with the permanent hearing loss and kidney damage that came with drugs like kanamycin.
The oral administration route makes a huge difference, too. When you’re not getting daily injections, you’re avoiding all the complications that come with them – injection site infections, the pain, the need for healthcare workers to administer them. Patients report better quality of life and actually stick with their treatment plans when they can take pills at home instead of travelling to clinics for shots. And because these drugs are more potent against resistant strains, you need fewer medications in your cocktail overall, which means fewer drug interactions and a lower chance of side effects piling up on each other.
What’s Next for TB Treatment?
The WHO is already working to update its treatment guidelines based on these new regimens, and you can expect these protocols to be rolled out globally within the next 12-18 months. Countries with high TB burdens, like India, South Africa, and the Philippines, are first in line for implementation. But here’s where it gets interesting – researchers aren’t stopping here.
Several pharmaceutical companies are now testing even shorter regimens that could bring treatment down to just four months instead of six. And the real game-changer? Scientists are exploring injectable formulations that you’d only need once a month, which could solve the adherence problem that’s plagued TB treatment forever. Your healthcare provider might soon have access to personalised treatment plans based on genetic testing of your specific TB strain, meaning no more one-size-fits-all approach. The pipeline looks promising, with at least three new drug candidates in Phase III trials right now… so if you’re dealing with drug-resistant TB, there’s genuine reason for optimism about what’s coming down the line.
Fact Box: The BPaL/BPaLM Treatment Regimen
The BPaL regimen is a revolutionary “all-oral” treatment that has transformed TB care from a two-year ordeal involving daily injections into a 6-month pill-based course.
| Feature | Technical Specification |
| The Drugs | Bedaquiline, Paretomanid, and Linezolid (plus Moxifloxacin for BPaLM). |
| Duration | Typically 6 months (26 weeks), extendable to 9 months if needed. |
| Success Rate | Approximately 89% to 91% in clinical trials (compared to 50–60% for older methods). |
| WHO Status | Primary recommended treatment for MDR-TB and Pre-XDR-TB as of 2026. |
| Key Advantage | No painful daily injections and a significantly lower “pill burden” for patients. |
To wrap up
Summing up, here’s what really stands out – you’re looking at treatment options that actually work against strains of TB that used to be nearly impossible to beat. These three approaches (bedaquiline, pretomanid combinations, and the BPaL regimen) aren’t just theoretical… they’re already saving lives in real-world settings. And the best part? You’re getting shorter treatment times with fewer side effects compared to the old multi-drug cocktails that could take years to complete.
Your healthcare provider now has genuine alternatives when standard TB medications fail. The data shows cure rates of 90% or higher in some studies, which is pretty incredible when you consider we’re talking about drug-resistant strains. But you’ll need to work closely with specialists who understand these newer protocols – because while these treatments are safer than older options, they still require careful monitoring. The takeaway for you is simple: drug-resistant TB isn’t the death sentence it once was, and medical science has finally caught up with tools that can actually make a difference in your outcome.
FAQ
Q: What makes these new tuberculosis treatments different from traditional TB medications?
A: Around 500,000 people develop drug-resistant TB every year, and the old treatment regimens were honestly pretty brutal – we’re talking 18 to 24 months of daily injections and pills with some nasty side effects. These three new approaches use only oral medications, which is huge because it means no more painful injections patients had to endure for months on end.
The treatment duration has been significantly cut down, too… some of these new regimens can work in as little as 6 to 9 months instead of the traditional 2 years. And here’s what really sets them apart – they’re specifically designed to target the mutations that make TB bacteria resistant to standard drugs. So instead of throwing the same old antibiotics at a problem that’s evolved past them, we’re actually using medications that can outsmart these resistant strains.
Plus, the side effect profiles are generally better tolerated. That matters because when people can actually stick with their treatment without feeling absolutely terrible, cure rates go way up.
Q: How effective are these new treatments compared to older drug-resistant TB therapies?
A: Clinical trials have shown success rates hovering around 85-90% for these newer regimens, which is a massive improvement over the 50-60% we were seeing with conventional treatments for multidrug-resistant TB.
But effectiveness isn’t just about whether the bacteria get killed off – it’s also about whether patients can actually complete the treatment. The older injectable-based regimens had dropout rates that were through the roof because people just couldn’t handle the side effects or the lifestyle disruption. These new all-oral options? Patient compliance has jumped significantly.
One of the regimens combines bedaquiline with pretomanid and linezolid, and in studies it cured about 90% of patients with extensively drug-resistant TB… that’s the really scary kind that doesn’t respond to most medications. Another approach using bedaquiline, pretomanid, moxifloxacin, and pyrazinamide showed similar success rates.
The real-world data is still coming in since these treatments are relatively new, but early results from countries that have adopted them show they’re living up to the clinical trial promises.
Q: Can anyone with drug-resistant TB access these new treatments, and are they affordable?
A: Access is definitely the tricky part here. While the WHO has recommended these regimens since 2018-2020, not every country has updated their national TB programs to include them yet. It varies wildly depending on where you live.
In terms of cost, there’s good news and bad news. The medications themselves have become more affordable through generic manufacturing and negotiated pricing for low and middle-income countries – we’re talking a few hundred to a couple thousand dollars for a full treatment course in many places. That’s still expensive, but way better than the $10,000+ that older regimens could cost.
The bigger barrier is often the healthcare infrastructure needed to properly diagnose drug-resistant TB in the first place. You need access to drug susceptibility testing, which isn’t available everywhere. And patients need monitoring throughout treatment to catch any side effects early.
So while these treatments exist and are becoming more accessible, there’s still work to be done to get them to everyone who needs them. Many international health organisations are working on expanding access, and several countries have already made these regimens their standard of care for drug-resistant cases.