How the AI Wearable for Addiction Recovery Detects Cravings
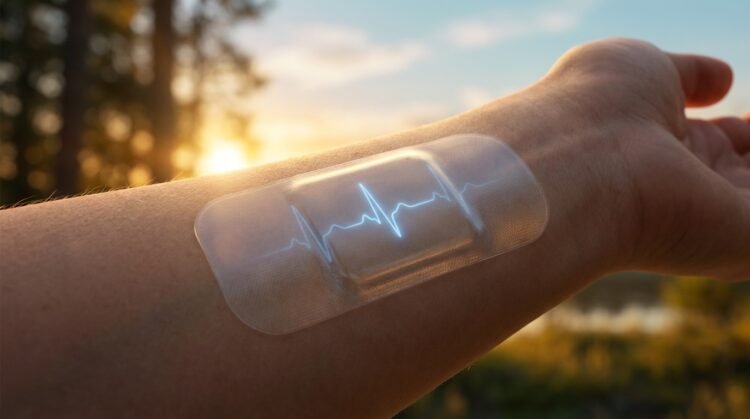
A groundbreaking AI wearable for addiction recovery is proving that technology might be our best ally in fighting intense cravings. Developed by researchers at Mass General Brigham, this “smart patch” uses biofeedback and artificial intelligence to detect stress and craving triggers before they spiral out of control. By monitoring heart rate variability in real time, the device prompts users to engage in breathing exercises at exactly the moment they are most vulnerable. The results are staggering: those using the AI wearable for addiction recovery were 64% less likely to use substances compared to traditional programs alone.
So, What’s the Deal with This Smart Patch?
The device at the centre of this research is called the Lief HRVB Smart Patch, and it’s basically like having a tiny stress detective sitting on your chest. You wear it throughout your day, and it’s constantly monitoring something called heart rate variability – which sounds technical but is actually your body’s way of showing how well you’re handling stress. When your HRV drops (meaning you’re getting stressed or experiencing cravings), the patch picks up on it before you might even fully realise what’s happening.

What makes this different from just tracking your heart rate on a fitness watch is the real-time intervention part. The patch doesn’t just collect data and show you pretty graphs later… it actually prompts you in the moment to take action. Think of it as an early warning system that taps you on the shoulder and says, “Hey, your body’s showing signs of stress right now, let’s deal with this before it becomes a problem.” For someone in recovery, that split-second awareness can make all the difference between riding out a craving and reaching for substances.
How Does It Work, Anyway?
Your heart rate variability is the variation in time between heartbeats, and when you’re stressed or experiencing cravings, that variability decreases. The smart patch monitors these changes continuously and uses AI to detect patterns that indicate you’re entering a high-risk state. Once it detects these warning signs, it sends you visual or auditory prompts via a connected app to guide you through controlled breathing exercises.
These aren’t just random breathing techniques either – they’re specifically designed to increase your HRV, which helps promote better emotional regulation and cognitive control. In the Mass General Brigham study, participants were asked to do at least 10 minutes of scheduled practice daily, plus an additional five minutes whenever the device prompted them. So you’ve got your regular maintenance breathing (like taking your vitamins), and then you’ve got the emergency intervention breathing when your body’s signalling trouble. The combination of both types of practice is what researchers believe makes the system so effective at interrupting the cycle of craving and substance use before it gains momentum.
Can It Really Help with Cravings?
The numbers from this study are pretty compelling, honestly. Out of 115 adults with severe substance use disorders in their first year of recovery, those who used the biofeedback device showed some significant improvements compared to the control group, who stuck with their regular recovery plans. Participants using the smart patch were 64% less likely to use substances on any given day during the eight-week study period. That’s not a small difference – we’re talking about nearly a two-thirds reduction in the likelihood of relapse on any particular day.
But it wasn’t just about whether they used substances or not. The device users also reported experiencing fewer negative emotions overall and had fewer cravings for alcohol or drugs throughout the study. David Eddie, the Mass General Brigham psychologist leading the research, explained that these devices can detect when people are stressed or experiencing cravings and “get out in front of risk” before it escalates. And that’s the key here – you’re not waiting until you’re in full-blown crisis mode to do something about it. You’re catching those early physiological signals and responding to them immediately with a proven intervention.
The first year of recovery is immensely challenging, as Eddie points out, and previous research has already shown that stress and low self-awareness of emotional states are major triggers for relapse during this vulnerable period. What this study demonstrates is that giving people a tool to become more aware of their internal states – and then immediately coaching them through a response – can actually interfere with that dangerous cycle. It’s not a cure-all, and nobody’s claiming it replaces other forms of treatment… but as an additional tool in your recovery toolkit? The evidence suggests it could be genuinely helpful for managing both short-term cravings and long-term stress management.
Why Stress Matters More Than You Think
Most people think about addiction as a chemical dependency issue, but your body’s stress response plays a much bigger role than you’d imagine. When you’re in that first year of recovery, stress isn’t just uncomfortable – it’s literally rewiring your brain’s craving pathways. And here’s what makes this so tricky: you might not even realise how stressed you are until you’re already reaching for something to take the edge off.
Your nervous system doesn’t distinguish between “good” stress and “bad” stress when it comes to triggering those old patterns. A job interview, a family argument, or even excitement about something positive can all flip the same biological switches. That’s why low self-awareness of emotional states becomes such a dangerous blind spot during recovery. You’re necessarily walking through a minefield without knowing where the mines are buried.
The Science Behind Stress and Addiction
The connection between stress and cravings comes down to something called heart rate variability, or HRV for short. Think of HRV as your body’s ability to shift gears smoothly – when it’s high, you’re adaptable and resilient. But stress and craving are linked to reduced HRV, which means your nervous system gets stuck in fight-or-flight mode. It’s like driving a car that can only go full speed or completely stopped… there’s no cruise control, no gentle acceleration.
What’s fascinating is that controlled breathing exercises can increase your HRV, which in turn promotes better emotional regulation and cognitive control. We’re not talking about some woo-woo meditation stuff here – this is measurable, physiological change. Modern HRV biofeedback devices can detect when your HRV drops and provide visual or auditory prompts to guide you through breathing adjustments. Previous research has already shown that this kind of biofeedback can help decrease anxiety and craving in people recovering from substance use disorders. So basically, your body’s telling you when a craving might be coming before your conscious mind even registers it.
My Take on Emotional Regulation
After looking at this research, I’m convinced that emotional regulation is the missing piece in most traditional recovery programs. You can go to all the meetings you want, but if you can’t recognise when your stress levels are creeping up, you’re always going to be playing defence. The Mass General Brigham study really drives this home – participants using the biofeedback device were 64% less likely to use substances on any given day. That’s not a small difference; that’s a game-changer.
What gets me excited about this approach is how it puts the power back in your hands. Instead of waiting until you’re in full-blown craving mode and trying to white-knuckle your way through it, you’re getting real-time data about what’s happening in your body. David Eddie from Mass General Brigham put it perfectly when he said this technology allows people to “get out in front of risk.” And honestly? That’s what recovery should be about – building awareness and skills, not just avoiding triggers.
The study participants were asked to do at least 10 minutes of scheduled practice daily and at least five minutes of prompted practice whenever the device detected elevated stress. Over those eight weeks, they reported their mood, cravings, and any substance use twice a day through their smartphones. The results showed participants who used the biofeedback device had fewer negative emotions and reported fewer cravings for alcohol or drugs. This intervention literally interfered with the cycle of craving and substance use before it could take hold. As Eddie noted, the first year of recovery is immensely challenging, and finding tools that help manage stress isn’t just about getting through that year – it’s about building skills that last a lifetime.
Real-Life Impact: What the Study Shows
So what actually happened when you put this technology in people’s hands for eight weeks? The Mass General Brigham team tracked 115 adults with severe substance use disorders – all of them navigating that incredibly difficult first year of recovery. Half received the Lief HRVB Smart Patch, while the other half continued their existing recovery plans, such as therapy sessions, support group meetings, or medication. Everyone checked in twice daily via smartphone to report how they were feeling, what they were craving, and whether they’d used any substances.

Your daily commitment wasn’t huge either. Participants were asked to do at least 10 minutes of scheduled breathing practice each day, plus an additional 5 minutes whenever the device prompted them because it detected stress signals. That’s it. Fifteen minutes total, broken up throughout your day, and the device does most of the heavy lifting by catching those stress spikes before you even fully register them yourself.
Numbers Don’t Lie – Less Craving, Less Use
Want to know if this thing actually works? Participants using the biofeedback device were 64% less likely to use substances on any given day compared to those following standard recovery protocols alone. That’s not a small difference – that’s the kind of number that makes researchers sit up and pay attention. And it wasn’t just about avoiding relapse… people wearing the patch reported experiencing fewer negative emotions overall and significantly reduced cravings for both alcohol and drugs throughout the eight-week study period.
What makes these findings particularly compelling is how they demonstrate the device actually interrupting the cycle before it spirals. You know that pattern – stress hits, cravings follow, and suddenly you’re fighting an uphill battle. The biofeedback intervention stepped in at that first domino, helping your body regulate stress through increased heart rate variability before cravings could take hold. The intervention interfered with the cycle of craving and substance use at its root, which is exactly what you need during that vulnerable first year when relapse rates are highest.
The Responses from Participants
Twice-daily check-ins gave researchers a real-time window into how people were actually doing – not just clinical measurements, but your actual lived experience. Participants reported their moods, what substances they were craving (if any), and whether they’d used anything since the last check-in. This constant feedback loop revealed something important: people using the smart patch consistently reported lower levels of negative emotions than the control group. That emotional regulation piece matters because negative feelings are often what trigger cravings in the first place.
The beauty of this approach is that it captured the messy reality of recovery as it was happening. You weren’t trying to recall how you felt last week during a therapy appointment – you were documenting it in the moment, twice every single day. This real-time data showed patterns that might otherwise get lost or minimised in traditional follow-up visits. When participants felt their stress rising or noticed a craving creeping in, many were already wearing a device that had detected those physiological changes and was guiding them through a breathing intervention before things escalated.
David Eddie, the Mass General Brigham psychologist leading the research, emphasised what this means for your long-term success: “The first year of recovery is immensely challenging. Our goal is to find tools that not only bridge people during that first year, but also help them manage their stress for the rest of their lives.” Because that’s really what you’re building here – not just a way to white-knuckle through early recovery, but actual skills and physiological responses that can support you indefinitely. The AI-powered prompts mean you’re learning to recognise and respond to stress signals in your body, vitally training yourself to intervene before cravings even fully form.
Can This Patch Change the Game for Recovery?
A 64% reduction in substance use on any given day – that’s not just promising, it’s potentially life-changing for people navigating their first year of sobriety. The Mass General Brigham study didn’t just show modest improvements… it demonstrated that a simple wearable patch could fundamentally disrupt the craving-to-relapse cycle that derails so many recovery journeys. And the beauty of it? You’re not adding another medication to your routine or committing to hours of therapy sessions – you’re wearing a device that works quietly in the background, intervening exactly when you need it most.
What makes this particularly exciting is the intervention’s real-time aspect. Traditional recovery tools ask you to recognise when you’re struggling and then take action, but that gap between awareness and response is exactly where relapse happens. This biofeedback patch flips that script entirely. It detects physiological changes in your heart rate variability before you’re even consciously aware that stress or cravings are building, then prompts you through breathing exercises that can pull you back from the edge. The AI-driven prompts mean you’re getting support in those critical moments – not hours later during your therapy session or days later at your recovery meeting.
What It Means for Those in Recovery
Your first year of recovery is statistically the most dangerous time you’ll face. But here’s something you might not realise – it’s not willpower that usually fails you, it’s your body’s stress response system. When your heart rate variability drops, you’re physiologically primed for poor decision-making, heightened emotional reactivity, and yes, intense cravings. The participants in this study who used the smart patch reported fewer negative emotions overall and significantly fewer cravings for alcohol or drugs throughout the eight-week period. That’s not just about avoiding relapse – that’s about actually feeling better day-to-day.
The study design itself tells you something important about how this fits into your existing recovery plan. Half the participants used only the patch, while the other half continued with their established recovery programs like meetings, therapy, or medication. This suggests the biofeedback device could work alongside whatever support system you’ve already built, not replace it. And with just 10 minutes of scheduled practice daily plus five minutes of prompted practice, you’re looking at a time commitment that fits into even the most hectic schedule. David Eddie, the psychologist leading the research, put it plainly – the goal isn’t just getting you through that first year, it’s giving you stress management tools that last a lifetime.
Here’s What We Still Need to Know
Phase 2 clinical trials are impressive, but they’re not the finish line. This study involved 115 adults with severe substance use disorders – a decent sample size, but we’re still talking about a relatively small group over just eight weeks. What happens at month six? Year two? Does the effectiveness hold up when you’re dealing with major life stressors like job loss, relationship problems, or health issues? And perhaps most importantly, will the results translate across different populations – different ages, socioeconomic backgrounds, types of substance use disorders?
There’s also the question of access and cost that the study doesn’t address. The Lief HRVB Smart Patch is a commercial device, which means it comes with a price tag that might put it out of reach for many people in recovery. Insurance coverage for biofeedback devices varies wildly, and if you’re already struggling financially (which many people in early recovery are), adding another expense – no matter how effective – might not be realistic. We need more data on long-term outcomes, larger and more diverse study populations, and, honestly, we need to figure out how to make this technology accessible to everyone who could benefit from it, not just those who can afford it.
The researchers also haven’t fully explored how this intervention works for people using medications for addiction treatment, or how it performs across different substances. Someone recovering from opioid use disorder might have a different physiological and psychological experience than someone recovering from alcohol use disorder. The study showed the patch interfered with the cycle of craving and substance use, but we still don’t know if certain substances or co-occurring mental health conditions might affect how well the biofeedback works. And what about people who’ve relapsed multiple times
Other Cool Tech Solutions in Addiction Treatment
Beyond the Patch – What Else is Out There?
Virtual reality therapy has been making waves in addiction treatment centres across the country, and honestly, it’s pretty wild to see someone put on a VR headset and work through their triggers in a controlled digital environment. You’re crucially stepping into scenarios that might normally send you spiralling – a bar, a party, even just a stressful work situation – but with your therapist right there guiding you through it. The tech lets you practice coping strategies in real time without any actual risk, and early studies are showing some really promising results for people dealing with alcohol and opioid dependencies.
Smartphone apps have also exploded onto the scene, though not all of them are created equal. Some of the better ones use AI to predict when you’re most vulnerable based on your patterns – maybe you always get cravings around 7 PM on Fridays, or when you’re in certain locations. These apps can send you personalised interventions right when you need them most, connecting you with peer support, guided meditations, or even your counsellor. And then there’s the fentanyl vaccine that’s heading into human trials in 2026… that’s a whole different ballgame. We’re talking about potentially blocking the drug’s effects at a molecular level, which could be a game-changer for preventing overdoses and supporting long-term recovery.
Blending Tech with Traditional Methods
What’s really exciting is watching treatment centres figure out how to weave these technologies into their existing programs without throwing the baby out with the bathwater. You’ve still got your recovery meetings, your one-on-one therapy sessions, maybe medication-assisted treatment – but now you’re also wearing a smart patch that’s monitoring your stress levels 24/7. The biofeedback device from the Mass General Brigham study worked alongside participants’ regular recovery plans, whether that was psychotherapy, recovery meetings, or medication. It wasn’t replacing anything… it was adding an extra layer of support that filled in the gaps between appointments.
Think about it this way – your therapist can only be there for an hour a week, but your cravings don’t stick to a schedule. That’s where tech steps in. The participants in the study were doing their regular recovery work AND using the smart patch, reporting their mood and cravings twice daily through their smartphones. This combination approach led participants to be 64% less likely to use substances on any given day, suggesting that tech works best when it supports, not replaces, the human connection that’s so vital to recovery. Because at the end of the day, you need both – the data-driven insights that catch you before you slip, and the human support that helps you understand why you were slipping in the first place.
Recovery programs are starting to see tech as another tool in the toolbox rather than a miracle cure. You might use your biofeedback device during the day to manage stress, then talk through what triggered those stress spikes with your counsellor later that week. Or you could practice your breathing exercises with the smart patch before heading into a high-risk situation you’ve been working through in therapy. It’s this back-and-forth between the digital and the personal that seems to be making the real difference, giving you round-the-clock support while still keeping that crucial human element front and centre.
The Future of Smart Devices in Mental Health
We’re standing at what feels like a turning point in how technology intersects with mental health treatment. The Mass General Brigham study isn’t just about one smart patch – it’s opening doors to a whole new approach where your recovery support system lives right on your body, tracking and responding to what you need in real time. Smart Patch Helps Addicts, Alcoholics Manage Stress and cravings through AI-powered interventions that previous generations could only dream about. What makes this particularly exciting is that participants were 64% less likely to use substances on any given day when using the biofeedback device – that’s not just statistically significant, that’s life-changing for people fighting to stay clean.
Beyond addiction recovery, you’re going to see these devices evolve into comprehensive mental health companions. Companies are already developing patches and wearables that can detect early warning signs of depression, anxiety attacks, and even PTSD episodes before you’re fully aware they’re happening. The technology that measures heart rate variability today could be monitoring cortisol levels, sleep patterns, and dozens of other biomarkers tomorrow… all working together to give you personalised interventions exactly when your body and mind need them most. And because the Lief patch showed that real-time AI prompts can interrupt the cycle of craving and substance use, we now have proof of concept that this approach actually works in the messiest, most challenging situations.
Are We Ready for More Wearable Tech?
That’s the million-dollar question, isn’t it? While the technology is advancing faster than most of us can keep up, there’s still a gap between what’s possible and what people are actually comfortable using. You’ve got privacy concerns – and they’re valid ones. Do you really want a device tracking your stress levels, emotional states, and potentially relapse triggers 24/7? Where does that data go, who has access to it, and what happens if your insurance company or employer gets their hands on information about your mental health struggles? These aren’t hypothetical worries… they’re real barriers that could slow adoption even when the devices themselves work beautifully.
But here’s what’s interesting about the Mass General Brigham trial: participants had to engage with the device for at least 10 minutes daily for scheduled practice and 5 minutes for prompted sessions. That level of commitment suggests that when you’re desperate for help, when you’re in that first year of recovery that David Eddie calls “immensely challenging,” you’ll absolutely use whatever tools give you a fighting chance. The dropout rate wasn’t mentioned in the study details, but the researchers’ clear results suggest that enough people stuck with it. So maybe we’re more ready than we think, especially when the alternative is relapse, continued suffering, or worse.
My Thoughts on the Direction We’re Headed
Honestly? I think we’re moving toward a future where mental health support becomes as personalised and responsive as your smartphone’s GPS. You wouldn’t dream of navigating a cross-country road trip without real-time traffic updates and route adjustments anymore – and soon, you won’t navigate recovery or mental health challenges without similar real-time guidance. The Lief patch is just the beginning. What excites me most isn’t even the technology itself, but what it represents: a shift from reactive mental health care to proactive intervention. Instead of waiting until you’ve already relapsed or hit rock bottom, these devices catch you on the way down and give you tools to course-correct.
The integration of AI into these wearables will be the game-changer that separates this generation of devices from anything that came before. Because it’s not just about collecting data – your Fitbit’s been doing that for years. It’s about having a system that learns your patterns, recognises when you’re deviating from baseline, and intervenes with personalised strategies that actually work for YOUR specific triggers and responses. The Mass General study showed that biofeedback reduced negative
Conclusion
Conclusively, imagine you’re six months into recovery and suddenly hit with an unexpected wave of stress at work or home – your heart starts racing, your mind goes to that familiar dark place, and the cravings come flooding back. This is where a smart patch could literally be a lifesaver. The Mass General Brigham study shows, pretty convincingly, that wearable biofeedback technology isn’t just a futuristic gimmick… It’s a practical tool that can actually interrupt that dangerous cycle between stress, cravings, and relapse. And the numbers speak for themselves – participants were 64% less likely to use substances on any given day. That’s huge when you’re talking about people in their most vulnerable first year of recovery.
But here’s what really matters for you or anyone you know struggling with SUD – this technology works because it catches you before you fall. Instead of waiting until you’re already in crisis mode, the patch detects physiological warning signs (like a drop in heart rate variability) and prompts you to do breathing exercises right then and there. It’s like having a recovery coach on your chest 24/7. Sure, it’s not going to replace therapy or support groups or whatever recovery plan you’ve got going, but it adds another layer of protection during those critical moments when relapse risk spikes. The first year of recovery is brutal, no way around that… so having AI-powered support that helps you manage stress in real time? That could make all the difference between staying on track and sliding backward.
FAQ
Q: How does a smart patch actually detect when someone is having cravings?
A: The technology is pretty fascinating when you break it down. These biofeedback patches monitor your heart rate variability (HRV), which basically measures the time between your heartbeats. When you’re stressed or experiencing cravings, your HRV drops – your heart rhythm becomes less variable and more rigid. The patch picks up on these changes in real time and uses AI to recognise the patterns that signal you’re in a vulnerable state.
Once it detects that drop in HRV, the device doesn’t just sit there collecting data… it actually prompts you to do breathing exercises right then and there. Think of it as having a recovery coach on your chest 24/7. The Mass General Brigham study showed this approach really works – participants who used the patch were 64% less likely to use substances on any given day compared to those who stuck with traditional recovery methods alone. And that’s huge when you’re talking about that critical first year of recovery.
Q: Do you have to wear the patch all day, and is it noticeable under clothing?
A: The Lief HRVB Smart Patch used in the study is designed to be worn continuously throughout your day. It’s a wearable device that sits on your chest, kind of like those heart rate monitor patches athletes use.
Most users report that it’s pretty discreet under regular clothing – you’re not walking around looking like you’re hooked up to medical equipment or anything. The study participants were asked to do at least 10 minutes of scheduled breathing practice daily, plus at least five minutes whenever the device prompted them because it detected stress or cravings. So yeah, you’re wearing it consistently, but the actual active intervention parts are short bursts throughout the day. It’s not like you need to stop everything and meditate for an hour. Just quick breathing exercises when your body signals it needs help regulating. That’s what makes it practical for real-world recovery – it fits into your actual life instead of requiring you to completely restructure your schedule around it.
Q: Is this patch meant to replace traditional recovery programs like therapy and meetings?
A: Absolutely not – and that’s an important distinction to make here. The researchers at Mass General Brigham designed this study to test whether the smart patch could work *alongside* existing recovery plans, not instead of them. Half the participants used the biofeedback device while the other half continued with their established recovery routines like 12-step meetings, psychotherapy, or medication-assisted treatment.
The patch is really more of an additional tool in your recovery toolkit. Dr David Eddie, the psychologist who led the research, specifically talked about finding tools that “bridge people during that first year” – meaning it’s meant to fill gaps and provide extra support during those moments when you can’t get to a meeting or call your therapist. Because cravings don’t wait for your next appointment, right? They hit you in the grocery store, at work, or at 2 am when you can’t sleep.
The study showed that this real-time intervention significantly reduced negative emotions and cravings. But it’s designed to complement therapy and other treatments, giving you an immediate response tool when stress and cravings spike unexpectedly. Think of it as backup support that’s always there, working with – not replacing – the human connections and professional help that are still vital to long-term recovery.