With growing evidence challenging the old “incidental finding” label, have you ever wondered why some Tarlov cysts suddenly become debilitating after years of silence? You might be surprised to learn that between 40% and 60% of symptomatic patients can trace their suffering to a specific traumatic event – whether it’s a hard fall, a lifting injury, or even the physical stress of childbirth. These fluid-filled sacs on your spinal nerve roots don’t just appear out of nowhere and start causing problems… there’s usually a trigger. And that trigger is often trauma. The “two-hit” hypothesis explains this perfectly: you’re born with a potential weak spot (first hit), then a traumatic event acts as the catalyst that converts a silent anatomical quirk into a source of severe neurological dysfunction (second hit). This synthesis examines how mechanical forces – from direct sacral impacts to chronic occupational strain – initiate the ball-valve mechanism that traps cerebrospinal fluid, creating relentless pressure that can erode bone and compress nerves. Understanding this trauma-cyst relationship isn’t just academic… It’s crucial for accurate diagnosis and treatment.
Key Takeaways:
- Unlike the old belief that Tarlov cysts are harmless incidental findings, we now know they’re actually dynamic and can become seriously problematic. Between 40% and 60% of people with symptoms can pinpoint a specific traumatic event – like a bad fall, childbirth, or even heavy lifting at work – as the moment everything changed. The “two-hit” hypothesis makes so much sense here… you’ve got a latent vulnerability (maybe you were born with weaker tissue in that area), and then trauma acts as the trigger that converts a sleeping cyst into an active problem.
The mechanics of how trauma kicks these cysts into gear is actually pretty fascinating. A direct impact on your tailbone creates shearing forces between nerve sheath layers, and that sudden spike in spinal fluid pressure can force CSF through tiny openings, inflating them into full-blown cysts. And here’s the kicker – the inflammation and scarring that follows the injury creates a restrictive “neck” on the cyst that sets up the ball-valve mechanism. So it’s not just the initial trauma… It’s what happens afterwards that really seals the deal.
Hemorrhage plays a bigger role than most people realise. Tarlov himself theorised that bleeding (often from trauma) was a key initiator, and modern evidence backs this up with hemosiderin deposits found in cyst walls – basically permanent markers of past bleeding. There are even documented cases of spontaneous brain hemorrhages causing blood to track down the spine and inflate previously silent sacral cysts. Blood breakdown products disrupt venous drainage, creating the perfect environment for fluid accumulation.
The chronic pressure inside these cysts doesn’t just cause pain… it literally remodels your bone structure. When fluid gets permanently trapped, and pressure builds up, it compresses the nerve fibres in the cyst wall and triggers something called sacral scalloping – where your bone actually erodes from the sustained pressure. This bony erosion is evident on imaging and is a telltale sign of a high-pressure, pathogenic cyst that’s been actively causing damage over time.
What Are Tarlov Cysts Anyway?
Figuring out the Basics
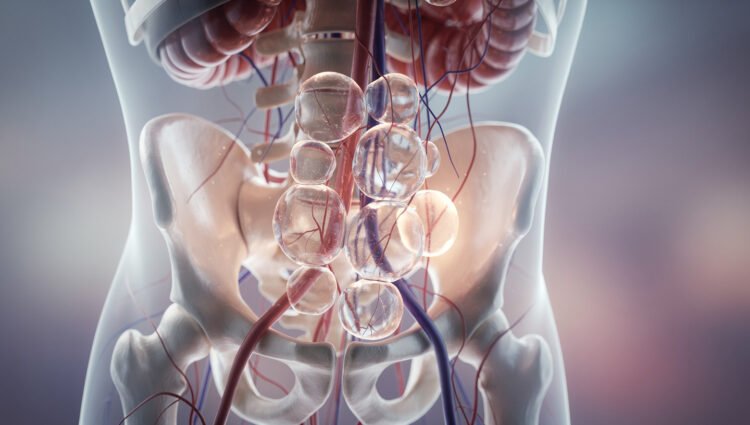
Picture this: you’re sitting in your doctor’s office, staring at an MRI report that mentions something called a “Tarlov cyst” on your sacral nerve roots. Your first thought? What the hell is that, and should I be worried? These fluid-filled sacs aren’t some exotic medical mystery – they’re actually sitting quietly in somewhere between 1.5% and 9% of the general population. Most people walk around their entire lives without ever knowing they have them. They form in a very specific spot: right at the junction where your dorsal root ganglion meets the posterior nerve root, nestled between two layers of your nerve sheath called the endoneurium and perineurium. Think of it like a water balloon that’s formed between the protective wrappings of your nerve fibres.
What makes a Tarlov cyst different from other spinal cysts is pretty straightforward – it actually contains nerve root fibres or ganglion cells within its wall or cavity. That’s the defining characteristic that distinguishes it from Type I meningeal cysts, which are simply fluid-filled pockets without neural tissue. The Nabors classification system puts Tarlov cysts squarely in the Type II category, and this distinction matters because those embedded nerve fibres are exactly why these cysts can cause such devastating symptoms when they decide to become problematic. While they can technically pop up anywhere along your spine, they have a clear favourite hangout spot: the S2 and S3 nerve roots in your sacrum. And here’s something that might surprise you – if you’re a woman reading this, you’re statistically more likely to develop symptomatic cysts, with some studies showing a 3:1 female-to-male ratio and patient surveys reporting that up to 86.6% of symptomatic individuals are women.
Why We Should Care About Them
So you might be thinking… if most of these cysts just sit there doing nothing, why all the fuss? Because when they do become symptomatic, they can absolutely wreck your life. Only a small subset – estimated between 1% and 22% – actually become clinically significant, but for those unlucky individuals, we’re talking about debilitating neurological symptoms that can include chronic pain, bladder and bowel dysfunction, sexual dysfunction, and progressive motor weakness. The real kicker is that for decades, doctors dismissed these as “incidental findings” – medical speak for “yeah, it’s there, but it doesn’t matter.” That perspective has done a massive disservice to patients who were suffering real, measurable neurological damage while being told their symptoms were all in their head or caused by something else entirely.
The shift in understanding these cysts as dynamic, progressive pathological entities rather than harmless anatomical quirks has been nothing short of revolutionary for patient care. What we now know is that between 40% and 60% of symptomatic patients can pinpoint a specific traumatic event that triggered their symptoms – a fall, a car accident, childbirth, or even something as mundane as lifting a heavy box at work. This isn’t a coincidence. These events represent the “second hit” in the two-hit hypothesis, where your pre-existing anatomical vulnerability (the “first hit”) gets activated by trauma that spikes your cerebrospinal fluid pressure and forces fluid into that vulnerable space. Once that ball-valve mechanism gets established – where fluid can flow in but can’t flow back out – you’ve got a ticking time bomb that will progressively enlarge, compress surrounding neural structures, and even erode the bone of your sacral canal over time.
The clinical implications of recognising this trauma-symptom connection are enormous. If you’re experiencing unexplained pelvic pain, sciatica, or neurological symptoms following an injury, and your doctor finds a Tarlov cyst on imaging, that’s not an incidental finding – that’s potentially your diagnosis. Understanding the pathophysiology means we can better predict which cysts are likely to become problematic, intervene earlier before irreversible nerve damage occurs, and validate the experiences of patients who’ve been told for years that their symptoms couldn’t possibly be related to “just a little cyst.”
The Trauma – Is It Really the Culprit?
What’s striking about the trauma-cyst connection isn’t that it exists… It’s that 40% to 60% of patients can pinpoint the exact moment their lives changed. We’re not talking about vague associations or statistical correlations that might mean something or might not. You’ve got people who can tell you the date, the time, sometimes even what they were wearing when they fell, lifted that box, or delivered their baby. And from that moment forward? Everything was different.
But here’s where it gets complicated. The other 40% to 60% of symptomatic patients can’t identify a specific traumatic event at all. So does that mean trauma isn’t the culprit? Not exactly. Because what we’re learning is that the “two-hit” model doesn’t require you to remember the second hit happening. Microtrauma – the kind you don’t even notice – can accumulate over years, gradually weakening those dural structures until one day, without any dramatic incident, the cyst suddenly becomes symptomatic. It’s like how you don’t notice a rope fraying until it finally snaps. The damage was happening all along; you just weren’t aware of it.
The Connection Between Injury and Cysts
The mechanical pathway from injury to cyst activation is surprisingly straightforward once you break it down. When you experience direct trauma to your sacral region – and we’re talking about falls onto your tailbone, car accidents, even aggressive chiropractic manipulations – the immediate spike in intrathecal pressure can force cerebrospinal fluid through microscopic weaknesses in your nerve sheath. Think of it like a water balloon with a tiny pinhole. Under normal pressure, nothing happens. But squeeze it hard enough, and suddenly that pinhole becomes a real problem. That’s necessarily what’s happening at the microscopic level in your sacrum during a traumatic event.
What makes this particularly insidious is the inflammatory response that follows. Your body’s trying to heal itself, right? But in doing so, it creates scar tissue and arachnoid proliferations that ultimately form the restrictive “neck” we talked about earlier. The very healing process establishes the ball-valve mechanism that traps fluid inside the cyst. It’s one of those cruel ironies where your body’s protective response actually sets up the chronic condition. And this isn’t speculation – histopathological studies of excised cyst walls consistently show evidence of past inflammation, hemosiderin deposits from old hemorrhages, and fibrotic tissue that’s characteristic of post-traumatic scarring.
Real-Life Stories That Back This Up
There’s this case that really drives the point home – a 52-year-old factory worker who’d been doing heavy lifting for decades without any major issues. Sure, he had some back stiffness here and there, but nothing that stopped him from working. Then one day, he bent down to lift a particularly heavy crate, felt something “give” in his lower back, and within weeks, he was experiencing severe perineal pain, bladder dysfunction, and sciatica that radiated down both legs. His MRI showed a massive Tarlov cyst at S2 that was eroding into the surrounding bone. The radiologist noted it was likely pre-existing but had been asymptomatic until the lifting incident. That single moment of increased intra-abdominal pressure during the Valsalva maneuver – that’s all it took to transform a silent anatomical variant into a disabling neurological condition.
Even more compelling is the 75-year-old woman who developed acute sacral radiculopathy following a spontaneous subarachnoid hemorrhage from a ruptured cerebral aneurysm. She’d never had any lower back or pelvic symptoms before. But after the hemorrhage, blood tracked down her spinal canal and was forced into a previously asymptomatic sacral cyst, causing it to expand rapidly. When they eventually operated, they found hemosiderin staining throughout the cyst wall – a permanent biological record of that hemorrhagic event. This case is particularly important because it demonstrates that you don’t even need external trauma. Internal hemorrhage, whether
How Trauma Turns Up the Heat
What’s fascinating – and honestly pretty unsettling – is that your body doesn’t just react to trauma in the moment. The initial injury triggers a cascade of biological responses that can persist for months or even years. When you think about trauma activating a Tarlov cyst, you’re probably picturing that single moment of impact… the fall, the car accident, the delivery room complication. But that’s just the opening act.
The real damage unfolds in the days and weeks that follow, as your body’s inflammatory response kicks into overdrive. Post-traumatic inflammation isn’t just swelling – it’s a complete remodelling of the tissue architecture around the nerve root. Cytokines flood the area, fibroblasts start laying down scar tissue, and arachnoid cells begin proliferating in ways they shouldn’t. This inflammatory “heat” creates the perfect storm for converting a harmless anatomical quirk into a pathological nightmare. And here’s the kicker: once this process starts, it often becomes self-perpetuating, even after the original injury has “healed” by conventional standards.
The Mechanics of Damage
Your sacral nerve roots weren’t designed to handle sudden mechanical stress. They’re delicate structures, protected by layers of tissue that are meant to glide smoothly against each other. When trauma strikes – whether it’s a direct blow to your tailbone or the explosive pressure surge from a violent sneeze – these layers get disrupted in ways that are surprisingly easy to visualise once you understand the anatomy. The shearing forces at the moment of impact can literally tear microscopic holes in the dural sleeve, creating communications that weren’t there before. Think of it like puncturing a water balloon that’s nested inside another balloon… suddenly you’ve got fluid where it doesn’t belong.
But the mechanical damage goes beyond just creating openings. The impact itself can stretch and deform the nerve root, causing immediate axonal injury to the nerve fibres embedded in the cyst wall. Studies using advanced imaging have shown that even seemingly minor trauma can cause up to 30% strain on sacral nerve roots – that’s enough to trigger cellular damage and death. Your nerve cells don’t bounce back from that kind of insult. They release inflammatory mediators, their myelin sheaths begin to break down, and the whole area becomes a biochemical war zone. The 52-year-old factory worker we mentioned earlier? His MRI showed not just cyst enlargement but also hyperintense signal changes in the surrounding nerve tissue – direct evidence of traumatic nerve injury that persisted long after the lifting incident.
Stress and Strain – The Unseen Forces
Most people don’t realise that some of the most damaging forces acting on your spine are completely invisible. You can’t feel them happening in real-time, and they don’t show up on standard imaging… but they’re there, working away every single day. Biomechanical stress isn’t about dramatic injuries – it’s about the cumulative effect of repetitive loading, postural strain, and the constant battle against gravity. Every time you bend forward, lift something, or even just stand up from a seated position, you’re creating pressure gradients within your spinal canal that can range from 5 to 50 mmHg above baseline.
What makes this particularly dangerous for someone with a latent Tarlov cyst is the Valsalva effect. When you strain – holding your breath while lifting, bearing down during bowel movements, or pushing during childbirth – your intrathecal pressure can spike to over 100 mmHg in less than a second. That’s more than enough force to drive CSF through any microscopic weakness in your dural sleeve. And if you’ve already got post-traumatic scarring, creating a one-way valve? Each Valsalva becomes a pumping action, progressively inflating the cyst like you’re working a bicycle pump. The insidious part is that these pressure spikes are so brief that you’d never connect them to your worsening symptoms… but your cyst is keeping score.
From Trauma to Trouble – What Happens Inside?
Between 40% and 60% of patients can pinpoint the exact moment their lives changed – the fall, the lift, the accident that transformed a silent anatomical quirk into a source of relentless pain. But what actually happens in those critical hours, days, and weeks after trauma strikes? Your body triggers a complex cascade of mechanical, inflammatory, and fluid-dynamic changes that can permanently alter the behaviour of a previously dormant cyst. Understanding this transformation isn’t just academic… It’s the key to explaining why some people develop devastating symptoms while others with identical-looking cysts on MRI remain completely pain-free.
The transition from asymptomatic to symptomatic isn’t a simple on-off switch. It’s more like a series of dominoes falling, where each mechanical insult triggers the next pathological change. The initial trauma creates both immediate structural damage and sets up the conditions for long-term progressive enlargement. And here’s what makes this particularly insidious – once the process starts, it often becomes self-perpetuating, driven by normal physiological forces like your heartbeat and posture that you can’t control.
Breaking Down the Pathophysiology
The moment of impact – whether it’s your tailbone hitting concrete or your spine compressing during a heavy lift – creates what researchers call a “hydrostatic spike.” Think of it like this: your spinal canal is filled with cerebrospinal fluid, and when trauma occurs, that fluid has to go somewhere. Studies show that intrathecal pressure can spike massively in milliseconds during impact trauma, reaching levels far beyond the normal 7-15 mmHg range. This sudden pressure surge acts like a hydraulic ram, forcing CSF through any microscopic weakness in the nerve sheath. If you’ve got that pre-existing vulnerability (the “first hit”), this pressure wave finds it and exploits it, forcibly dilating what was maybe just a tiny potential space into an actual fluid-filled cavity.
But the mechanical damage is only part of your body’s response. The trauma also triggers an inflammatory cascade that’s actually more important for long-term cyst behaviour than the initial injury itself. Your immune system floods the area with inflammatory mediators, causing local edema and triggering the proliferation of arachnoid cells. This inflammation leads to scarring – and here’s where things get really problematic. That post-traumatic scar tissue forms around the cyst’s opening, creating a restrictive “neck” that acts like a one-way valve. The 52-year-old factory worker mentioned earlier? His cyst wall biopsy showed dense fibrous tissue at the ostium, a permanent structural change that happened in the weeks following his lifting injury. This scarring doesn’t heal or resolve… it becomes a permanent anatomical feature that traps fluid and establishes the mechanical conditions for progressive enlargement.
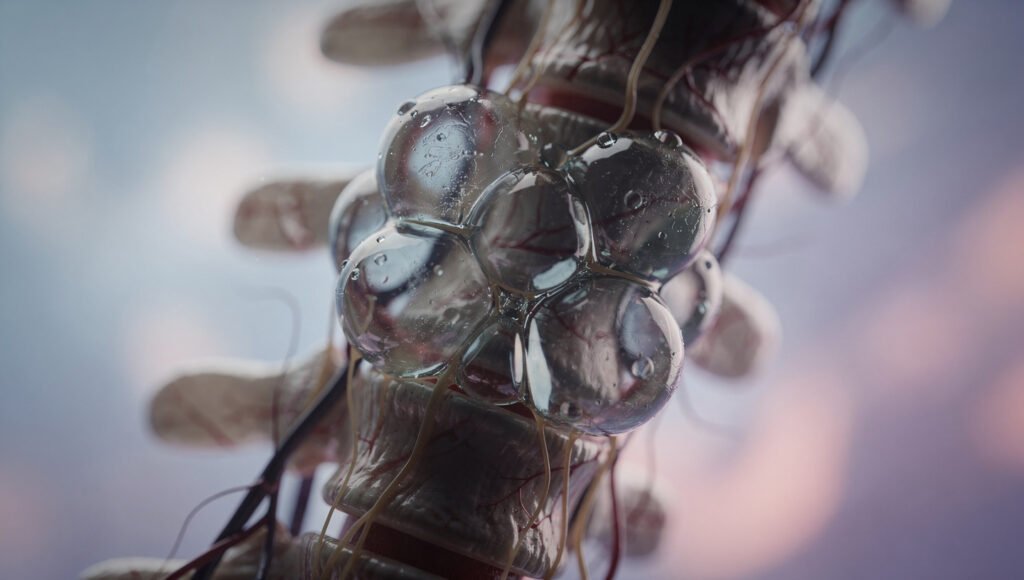
The Ball-Valve Mechanism – What’s That?
Your heart beats roughly 100,000 times per day, and with each beat, it’s potentially pumping more fluid into your cyst. The ball-valve mechanism explains why Tarlov cysts don’t just fill up once and stop – they continue growing relentlessly over months and years. During cardiac systole, when your heart contracts and sends a pressure wave through your vascular system, that wave also pulses through your cerebrospinal fluid. This pulsatile force pushes a small amount of CSF through the cyst’s opening during each heartbeat. But here’s the trap: during diastole, when pressure drops, that post-traumatic scarring or an arachnoid flap acts like a check valve, snapping shut and preventing the fluid from flowing back out.
It’s a ratchet effect, really – one tiny increment of fluid enters with each cardiac cycle, and none leaves. Over time, this creates a pressure differential in which the cyst’s internal pressure exceeds the pressure of the surrounding thecal sac. This chronic hypertension is what drives the most devastating pathological consequences: direct compression of the nerve fibres embedded in the cyst wall, mass effect on adjacent nerve roots, and even erosion of the surrounding sacral bone. Radiologists call this bone erosion “sacral scalloping,” and when you see it on imaging
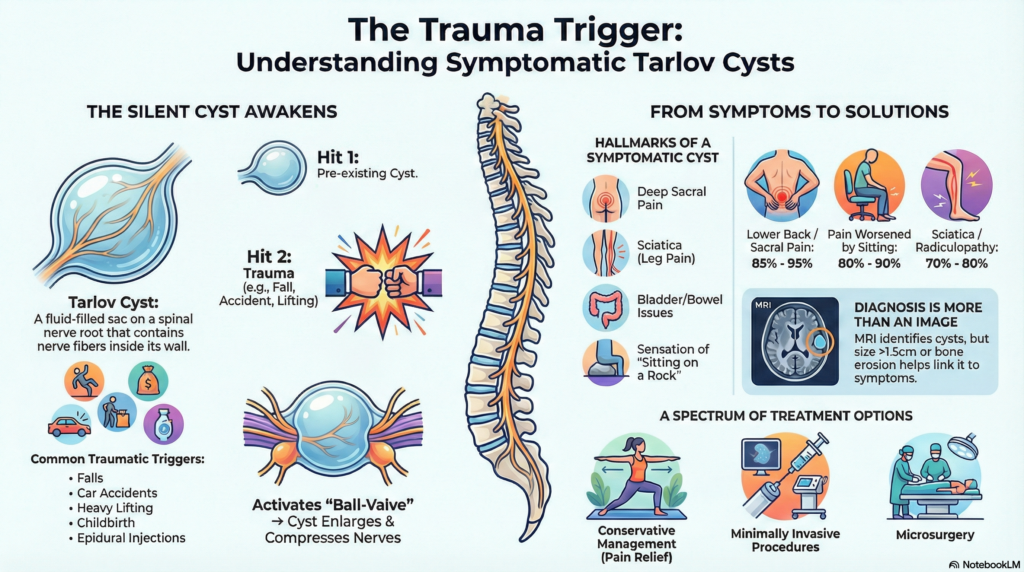
Symptoms and Signs – How Do You Know?
Your body has a way of sending distress signals when something’s seriously wrong, and with symptomatic Tarlov cysts, those signals can be maddeningly vague at first… until they’re not. What makes these lesions particularly challenging is that your symptoms can mimic dozens of other conditions, from herniated discs to fibromyalgia, leading to years of misdiagnosis and frustration. The clinical presentation typically involves pain that radiates from your lower back or sacrum down into your legs, often accompanied by strange sensations like burning, tingling, or that “pins and needles” feeling that won’t quit. But here’s where it gets tricky – the symptoms aren’t always consistent. You might have good days and terrible days, and this variability often leads doctors to dismiss your complaints as psychosomatic or stress-related.
The constellation of symptoms you experience directly correlates with which specific nerve roots are being compressed by your cyst. Because these lesions most commonly occur at S2 and S3, you’ll often notice problems with bladder and bowel function – things like urinary urgency, incomplete emptying, or constipation that suddenly becomes a major issue. Sexual dysfunction is another frequently reported symptom that patients are often reluctant to discuss, but it is actually a significant red flag. Pain patterns can be positional, meaning sitting might be absolutely unbearable while standing provides relief, or vice versa, depending on how the cyst shifts with posture and how fluid dynamics change throughout the day. According to comprehensive case reviews, including this (PDF) Symptomatic Tarlov cyst: Report and review, the average time from symptom onset to correct diagnosis can span several years, during which you might undergo multiple ineffective treatments for conditions you don’t actually have.
Spotting the Red Flags
Certain warning signs should immediately elevate your concern and prompt aggressive investigation. Progressive neurological deficits are the biggest red flag – if you’re noticing increasing weakness in your legs, foot drop (where you can’t lift the front part of your foot), or worsening numbness that’s spreading rather than staying localised, you need imaging now, not later. Saddle anesthesia, which is numbness in the area that would contact a saddle if you were riding a horse (your inner thighs, buttocks, and perineum), represents a neurological emergency because it suggests significant compression of the sacral nerve roots that control bowel, bladder, and sexual function. And if you develop what’s called cauda equina syndrome – a combination of severe lower back pain, bilateral leg weakness, saddle anesthesia, and loss of bladder or bowel control – you need emergency neurosurgical evaluation because permanent nerve damage can occur within hours to days.
But the red flags aren’t always that dramatic or acute. Sometimes, they’re more insidious patterns that emerge over months or years. You might notice that your symptoms have a clear temporal relationship to a specific traumatic event – maybe you fell on your tailbone six months ago and the pain just never resolved, or perhaps you had a difficult childbirth, and since then you’ve had this constellation of pelvic pain, bladder issues, and leg pain that no one can explain. Positional pain that’s dramatically worse with sitting or standing is particularly suggestive of a Tarlov cyst rather than a herniated disc, because hydrostatic pressure changes with posture directly affect cyst pressure and, in turn, nerve compression. If you’re also experiencing headaches that worsen when upright and improve when lying down, this could indicate a CSF leak or a pressure imbalance related to your cyst pathology. Importantly, some patients develop a low-pressure headache syndrome alongside their sacral symptoms.
Personal Accounts That Shine Light on Symptoms
Real patient experiences often capture the lived reality of this condition better than any medical textbook can. Take Sarah, a 42-year-old teacher who spent three years being told her symptoms were “just stress
Treatment Options – What Can You Do?
So you’ve been diagnosed with symptomatic Tarlov cysts, and now you’re sitting there wondering what comes next. The treatment landscape for these lesions isn’t exactly straightforward – and honestly, that’s because we’re dealing with a condition that only recently started getting the clinical attention it deserves. Your treatment path will depend heavily on the severity of your symptoms, the size and location of your cysts, and whether they’re actively causing nerve compression or bone erosion. Some patients find relief through conservative management, while others require surgical intervention to prevent further neurological damage.
The reality is that there’s no one-size-fits-all approach here. Conservative treatments like pain management, physical therapy modifications, and activity restrictions work for some people – particularly those with mild to moderate symptoms. But if you’re experiencing progressive neurological deficits, bowel or bladder dysfunction, or evidence of significant sacral scalloping on imaging, you might be looking at surgical options. The most established surgical technique involves microsurgical cyst fenestration with fibrin glue sealing, with success rates of 60-80% in experienced hands. Some surgeons also perform cyst wall resection or imbrication to collapse the cyst cavity. The key thing to understand is that surgery isn’t a guaranteed cure, and recurrence rates can range from 10-30% depending on the technique used and whether the underlying ball-valve mechanism is adequately addressed.
Making Sense of Your Choices
Deciding between conservative management and surgery can feel overwhelming, especially when you’re dealing with chronic pain that’s affecting every aspect of your life. Here’s what you need to weigh: conservative approaches make sense if your symptoms are manageable and not progressing. This might include NSAIDs for pain control, avoiding activities that increase intrathecal pressure (heavy lifting, high-impact exercise, straining), and working with a physical therapist who understands sacral nerve root pathology. Some patients benefit from CT-guided cyst aspiration combined with fibrin glue injection – a minimally invasive option that can provide temporary or sometimes lasting relief. But the catch? Aspiration alone has high recurrence rates (often 50% or more) because it doesn’t address the underlying valve mechanism that keeps fluid from being pumped back in.
Surgery becomes the more compelling option when conservative measures fail or when you’re facing progressive neurological deterioration. And this is where things get tricky – you need to find a neurosurgeon who actually has experience with Tarlov cysts, because they’re rare enough that many surgeons have never operated on one. The surgical goal is threefold: decompress the affected nerve roots, eliminate the ball-valve mechanism of inflow, and prevent recurrence. Techniques vary, but the most successful approaches involve opening the cyst, evacuating the fluid, identifying and closing the communication with the thecal sac, and then using fibrin glue to seal everything. Some surgeons will also perform a laminectomy to give the nerve roots more room. What you’re really deciding is whether the potential benefits – which can include significant pain reduction and halting of neurological decline – outweigh the surgical risks, such as CSF leak, infection, or nerve injury during the procedure.
The Road to Relief – What to Expect
If you go the surgical route, you should know upfront that recovery isn’t quick or linear. Most patients spend 3-5 days in the hospital post-operatively, and you’ll likely need to maintain strict bed rest for the first week or two to allow the fibrin seal to solidify and prevent CSF leakage. The immediate post-op period can actually be rough – some patients experience a temporary worsening of symptoms due to surgical inflammation and manipulation of already irritated nerve roots. But here’s what the data shows: patients who respond well typically start noticing improvement around the 6-week mark, with continued gains over 3-6 months as inflammation resolves and nerves recover from chronic compression.
Pain reduction is usually the first improvement you’ll notice, followed by a gradual return of sensation and motor function if those were affected. Bowel and bladder symptoms can be slower to resolve and may not fully normalise if the nerves were compressed for an extended period before surgery.
Conclusion
So what does all this evidence really mean for your understanding of Tarlov cysts? From above, you can see that the relationship between trauma and symptomatic Tarlov cyst disease isn’t just a coincidence reported by patients – it’s a well-supported, mechanistically sound pathway that transforms dormant anatomical variants into sources of profound neurological suffering. The “two-hit” model gives you a framework that makes sense of why some people carry these cysts silently for decades while others experience sudden, devastating symptom onset after a fall, a difficult childbirth, or even years of occupational strain. When 40% to 60% of symptomatic patients can point to a specific traumatic event as their turning point, you’re looking at a signal that’s too strong to dismiss as mere correlation.
Your takeaway here should be clear. Trauma – whether it’s a single high-impact event, chronic mechanical stress, or internal hemorrhage – acts as the critical catalyst that initiates the ball-valve mechanism and sets off a self-perpetuating cycle of cyst expansion and neural damage. This isn’t a static condition you can wait out. Once that valve forms and CSF starts accumulating under pressure, you’re dealing with a progressive pathology that erodes bone, compresses nerves, and resists conservative management. And here’s what matters most for your clinical practice or your own health journey: recognising this traumatic trigger means you can potentially identify at-risk patients earlier, validate the experiences of those whose symptoms appeared “out of nowhere” after an injury, and advocate more aggressively for imaging and intervention before irreversible neural damage occurs. The evidence synthesised in this paper should fundamentally change how you view these lesions – not as incidental findings, but as trauma-activated diseases that demand your attention and respect.
FAQ
Q: Can a car accident or a bad fall really cause my Tarlov cyst symptoms, or is that just a coincidence?
A: Between 40% and 60% of people with symptomatic Tarlov cysts can pinpoint the exact traumatic event that started their nightmare – and that’s not a coincidence, that’s clinical evidence. When you fall hard on your tailbone or get rear-ended in a car crash, the sudden impact creates what researchers call a “hydrostatic spike” – basically a massive pressure wave that forces cerebrospinal fluid into a vulnerable spot in your nerve sheath. Think of it like this… You might’ve been born with a tiny weak spot (the “first hit”), but it just sat there doing nothing until that fall or accident came along as the “second hit” and BAM, suddenly fluid gets pumped in, and you’ve got a cyst that won’t stop growing.
And here’s what makes it even more frustrating – the trauma doesn’t just create the cyst, it often sets up this awful ball-valve mechanism where fluid keeps getting pumped in with every heartbeat but can’t get back out. The injury causes inflammation and scarring that acts like a one-way door. So even though the accident happened months or years ago, you’re still getting worse because that valve is still trapping fluid. This is why so many people get dismissed by doctors who say “it’s just an incidental finding” – but if your symptoms started right after trauma, that’s your body telling you the real story.
Q: I’ve been doing heavy lifting at work for years and just developed Tarlov cyst symptoms – could my job actually be responsible for this?
A: Your job might’ve been setting you up for this for a long time, and that last heavy lift was just the final straw. There’s actually a documented case of a 52-year-old factory worker who had years of spinal strain and then lifted one heavy object that triggered severe Tarlov cyst symptoms – sound familiar? What happens is this: when you lift something heavy, you naturally do what’s called a Valsalva maneuver (basically holding your breath and straining), and this dramatically spikes the pressure in your abdomen and spine. That pressure acts like a pump, forcing cerebrospinal fluid into any weak spots.
So you’ve got this double whammy situation. Years of repetitive lifting and mechanical stress gradually weaken the structures around your sacral nerve roots, leaving them vulnerable. Then one day, you lift that particularly heavy box or awkward piece of equipment, and your intrathecal pressure shoots up, forcing fluid into a space it shouldn’t be. The cyst that might’ve been sitting there, tiny and asymptomatic for years, suddenly gets inflated like a balloon, and now it’s pressing on nerve fibres and causing all your symptoms.
Because this develops gradually with a sudden tipping point, a lot of workers’ comp claims get denied – but the connection is real and documented in medical literature.
Q: Why do Tarlov cysts keep getting worse over time, even though my original injury happened years ago?
A: This is the really insidious part that makes Tarlov cysts so frustrating to live with – the original trauma might be long gone, but it set up a self-perpetuating cycle that keeps making things worse. When that initial injury happened, it didn’t just create the cyst… it also triggered inflammation and scarring that formed what doctors call a “ball-valve mechanism.” Essentially, your body created a one-way valve that lets cerebrospinal fluid flow INTO the cyst but prevents it from flowing back OUT.
Here’s what’s happening inside you right now: with every single heartbeat, the pressure wave from your cardiac cycle pushes a tiny bit of CSF through that valve into your cyst. During the relaxation phase between heartbeats, the valve closes – maybe because of scar tissue from your old injury, or an arachnoid flap that formed afterwards. So drip by drip, beat by beat, your cyst is getting pumped up with more fluid that has nowhere to go. Over months and years, this causes the cyst to expand, the pressure inside it to build, and eventually it starts eroding the bone around it (that’s the “sacral scalloping” you might see on MRI reports).
This is why your symptoms can start mild and become debilitating
References
1. Symptomatic Tarlov Cyst Following Spontaneous Subarachnoid
https://pmc.ncbi.nlm.nih.gov/articles/PMC3206274/
2. Management of Tarlov cysts: an uncommon but potentially serious spinal column disease—review of the literature and experience with over 1000 referrals – PMC – PubMed Central, https://pmc.ncbi.nlm.nih.gov/articles/PMC10761484/
3. Tarlov IM. Perineurial cysts of the spinal nerve roots. Arch Neurol Psychiatry. 1938;40:1067–74.
4. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, Rizzoli HV. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68(3):366–77.
5. Neulen A, Kantelhardt SR, Pilgram-Pastor SM, et al. Microsurgi-cal fenestration of perineural cysts to the thecal sac at the level of the distal dural sleeve. Acta Neurochir. 2011;153:1427–34.
6 Post-Traumatic Haemorrhagic Tarlov’s Cyst: a Case Report and …, https://flore.unifi.it/retrieve/29dfc9eb-d62e-4414-86a3-e032540f4c39/SN%20Compr%20Clin%20Med%202023.pdf
7. Post-traumatic hemorrhage in a large sacral Tarlov cyst causing …, https://mss-ijmsr.com/post-traumatic-hemorrhage-in-a-large-sacral-tarlov-cyst-causing-acute-radiculopathy/