Understanding Grover Disease: A Comprehensive Guide to Diagnosis, Management, and Empowerment
Key Takeaways
- Grover disease, or transient acantholytic dermatosis, often masquerades as common rashes and requires biopsy for definitive diagnosis.
- Triggers include heat, sweating, sun exposure, prolonged bed rest, certain medications, and dry air.
- Treatment is layered: gentle skin care, topical corticosteroids, antihistamines, and, when needed, phototherapy or systemic agents.
- Personalized trigger avoidance and lifestyle adjustments are crucial to minimize flares and improve quality of life.
- Emerging therapies like dupilumab offer hope for refractory cases, highlighting the importance of tailored dermatologic care.
Table of Contents
- Introduction
- Core Concepts & Mechanisms
- Epidemiology and Clinical Features
- Diagnosis and Histology
- Treatment & Management Approaches
- Prevention & Practical Applications
- Conclusion & Future Outlook
- FAQ
- Further Reading
Introduction
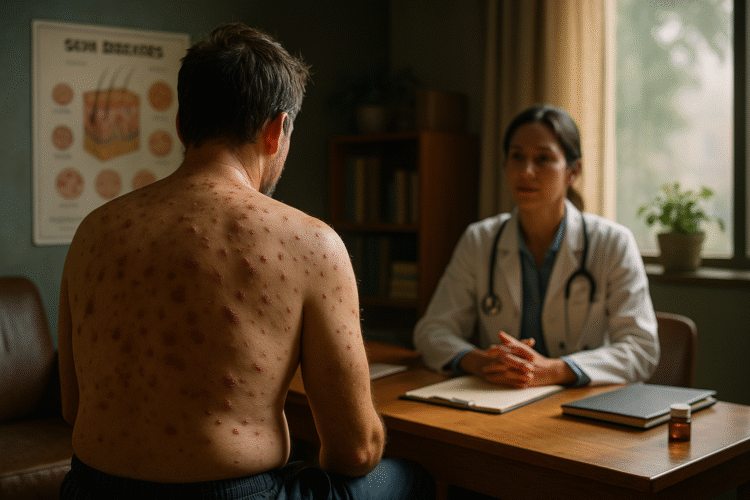
At first, Mark thought it was just a heat rash. He’d been helping his daughter move apartments on a steamy July weekend, and the next morning he woke up with a crop of tiny, red, itchy bumps across his chest and upper back. No big deal, he figured. He slathered on a little over-the-counter hydrocortisone, switched to a lighter T-shirt, and got on with his day.
But the itch was relentless. Not the faint, background kind—the kind that hijacks your focus. It kept him awake at night. It flared after showers, after quick walks, even after sitting in the sun during his grandson’s baseball game. Weeks stretched into months. Every time it cooled off, it seemed to come roaring back. His primary care doctor called it contact dermatitis. Then eczema. Then maybe some kind of folliculitis. Several creams later, nothing was really better. That’s when a dermatologist suggested a small skin biopsy.
The result? Grover disease.
If you’re hearing that name for the first time, you’re not alone. Grover disease—also called transient acantholytic dermatosis—is a rare, often underdiagnosed skin condition that tends to surprise people the first time they meet it. “Transient” sounds reassuring, but it can be misleading. For many, the rash does eventually settle down. For others, it lingers, recurs, or even becomes a long-term visitor that’s stubbornly difficult to evict.
It tends to show up on the trunk—the chest, back, maybe the shoulders and upper arms—and typically affects middle-aged to older adults, especially men. Even though it’s considered rare—prevalence is estimated around 0.1%—experts believe it’s underreported, in part because it masquerades as more familiar conditions and often never gets biopsied.
In the sections ahead, we’ll cover:
- What Grover disease is and isn’t
- Why it’s under-appreciated clinically
- Key triggers and how to avoid them
- Diagnostic tips and histologic hallmarks
- Layered treatment and lifestyle strategies
- Emerging therapies and future directions
Core Concepts & Mechanisms
What exactly is Grover disease?
Named after Dr. Ralph Grover (1970), this condition features clusters of small, itchy, red, sometimes crusted or blister-like bumps on the chest and back. Under the microscope, pathologists see acantholysis—keratinocytes (the “bricks” of the epidermis) losing their connections, like mortar dissolving between bricks.
Transient acantholytic dermatosis suggests many cases burn out within weeks to months. But some recur seasonally or become chronic, affecting quality of life for years.
Who tends to get it?
- Middle-aged and older adults, with a male-to-female ratio of about 2:1 to 3:1
- People with lighter skin are reported more often (likely a biopsy bias)
- Estimated prevalence around 0.1%, though underrecognition is common
Clinical Presentation
- Small, intensely itchy red bumps (papules), sometimes with crusting or tiny blisters
- Favorite territory: central chest, upper back, shoulders, upper arms
- Itch severe enough to disrupt sleep and concentration
Key Triggers
- Heat & Sweating: Persistent moisture and friction weaken cell adhesion
- Sunlight & Radiation: UV and ionizing rays stress adhesion proteins
- Prolonged Bed Rest: Trapped heat, pressure, microtrauma in immobile skin
- Medications: Certain chemotherapy and post-transplant drugs
- Dry Air: Low humidity makes the skin barrier brittle
Epidemiology and Clinical Features
Grover disease most often appears in men over 50, though cases in women and younger adults occur. While many flares resolve within weeks to months, some become chronic or recurrent, especially with ongoing triggers.
Diagnosis and Histology
When to biopsy: Persistent, recurrent, or treatment-resistant rashes should prompt a skin biopsy for definitive diagnosis.
- Histology: Acantholysis, sometimes dyskeratosis, mixed Darier- or Hailey-Hailey-like patterns, superficial inflammation
- Immunofluorescence: Typically negative, helping rule out autoimmune blistering diseases
Treatment & Management Approaches
Management is multilayered: soothe the skin, reduce inflammation, restore the barrier, and prevent triggers.
1. Soothing Skin Care
- Fragrance-free, gentle cleansers
- Lukewarm, brief showers; finish with a cool rinse if tolerated
- Thick, fragrance-free moisturizers within three minutes of drying
- OTC anti-itch lotions (menthol, pramoxine, camphor)
2. Anti-inflammatory Treatments
- Topical corticosteroids (medium to high potency during flares; taper carefully)
- Topical calcineurin inhibitors as steroid-sparing options
- Oral antihistamines for itch relief (sedating at night, non-sedating by day)
3. Phototherapy
Narrowband UVB may help when topicals are insufficient, using controlled doses under dermatology supervision.
4. Systemic Options
- Oral retinoids (acitretin, isotretinoin) for recalcitrant cases; monitor labs and pregnancy status
- Short courses of systemic steroids for severe flares
- Off-label dupilumab in select refractory patients
Prevention & Practical Applications
Understanding and avoiding your personal triggers is key. Practical strategies include:
- Cool your microclimate: Fans, cool rooms, layered breathable bedding
- Dress wisely: Moisture-wicking, lightweight fabrics; avoid tight or scratchy materials
- Manage sweat: Exercise in cooler times, rinse and re-moisturize after sweating
- Protect from sun: UPF clothing, shade, mineral sunscreen on unaffected areas
- Shower smart: Lukewarm water, moisturize immediately
- Winter care: Use a humidifier, switch to richer emollients
- Hospital tips: Moisture-wicking sheets, frequent repositioning, cool environment
Conclusion & Future Outlook
Grover disease may hide in plain sight, but once recognised, it’s highly manageable. Early biopsy, layered treatment, trigger avoidance, and emerging therapies empower patients to reclaim comfort. With growing awareness and targeted strategies, the path from confusion to control is shorter than ever.
Your next steps: Talk to your dermatologist about biopsy if your rash is persistent. Start cooling and gentle-care routines today. Track flares and triggers. Implement the personalized plan that lets you live itch-free.
FAQ
Is Grover disease contagious?
No. It cannot be transmitted between people.
How long does a flare last?
Most flares resolve within weeks to months. Some recur seasonally or become chronic without trigger control.
Will topical steroids cure Grover disease?
They reduce inflammation and itch but are part of a broader management plan—they don’t “cure” the underlying acantholysis.
Can I use phototherapy if sun triggers my rash?
Yes. Controlled narrowband UVB under medical supervision can help, despite natural sun being a trigger.
What lifestyle changes help most?
- Keeping skin cool and dry
- Adjusting shower temperature and duration
- Wearing breathable fabrics
- Tracking triggers in a simple diary
Further Reading
- 7 Trauma Healing Practices – Science-Backed Mind-Body Healing
- Understanding the Spectrum of Alcohol Use Disorder: A Practical Guide for Clinicians
- The Real Reasons Behind Your Constant Hunger – Hormonal Insights
- Understand Chronic Kidney Disease: Causes, Symptoms and Management
- Why Young People Should Care About the Fight-or-Flight Response
“`